Author Interviews, Medical Imaging / 05.12.2024
AI-Enhanced Routine Abdominal CT Scans Detected Cardiovascular Disease Risk
MedicalResearch.com Interview with:
Miriam A. Bredella, MD, MBA
Bernard and Irene Schwartz Professor of Radiology & Vice Chair for Strategy
Associate Dean for Translational Science
Director, Clinical and Translational Science Institute
NYU Grossman School of Medicine
NYU Langone Health
Translational Research Building 743
New York, NY 10016
MedicalResearch.com: What is the background for this study?
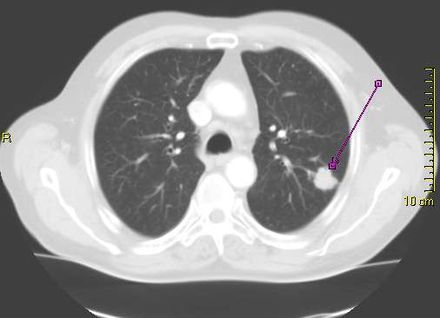
Response: We perform >80 million CTs every year in the US, and there is a lot of information on these CTs that is not used and “thrown away.” Opportunistic imaging or opportunistic screening with the help of AI takes advantage of this information and automatically detects and quantifies vascular calcification, bone mineral density, abdominal fat or muscle mass. In our study, we wanted to detect whether calcification of the abdominal aorta, quantified using AI, could predict coronary artery calcification and major cardiovascular events (e.g. myocardial infarction, cardiac revascularization, stroke, or death).
(more…)