MedicalResearch.com Interview with:
 Jagadeesh BAYRY, DVM, PhD, HDR
Jagadeesh BAYRY, DVM, PhD, HDR
Scientist CRCN/Associate Professor-INSERM
Institut National de la Santé et de la Recherche Médicale (INSERM) Unité 1138
Centre de Recherche des Cordeliers
PARIS , FRANCE
MedicalResearch.com: What is the background for this study? What are the main findings?
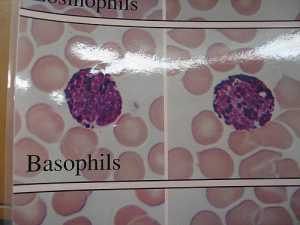
Response: Basophils are rare granulocytes that are important for the protection against helminth parasites. In addition, basophils mediate T helper 2 responses, support B cell differentiation, and thus establish a vital link between innate and adaptive immunity. Although rare in number, basophils are implicated in various pathological conditions due to the fact that they undergo rapid activation in response to a wide range of stimuli they receive. These stimuli induce the release of diverse immune mediators including cytokines and mediators of hypersensitivity reactions histamine and leukotriene. Basophils are well known for their pathogenic role in allergic diseases. Recent data also advocate basophils in the pathogenesis of autoimmune and other inflammatory diseases. Therefore, considering the impact of dysregulated functions of basophils on the immune response in various diseases, we deliberated that it is essential to understand the regulatory mechanisms by which basophils are kept in check.
Among immunoregulatory cells, CD4
+CD25
+FoxP3
+ regulatory T cells (Tregs) have been widely studied for their role in immune tolerance and in the maintenance of immune homeostasis. Tregs modulate autoimmune and inflammatory responses by exerting direct suppressive effects on various immune cells including dendritic cells, T cells, macrophages, monocytes, B cells, neutrophils, natural killer cells, and mast cells. In view of emerging reports on the role of basophils in various pathological conditions, we investigated if Tregs are able to control the activation and functions of basophils.
In contrast to the central dogma on Tregs as immunosuppressors, we discovered that human basophils are refractory to Treg-mediated suppression. On the contrary, we found that Tregs stimulate resting basophils to induce the expression of activation markers CD69, CD203c, and CD13, and release cytokines IL-4, IL-8, and IL-13. Treg-induced activation of basophils involves IL-3 and STAT5 but was not contact-dependent. These results provide evidence of direct positive effects that human Tregs have on basophil activation and reveal a previously unrecognized feature of this cell subset well known for immunosuppressive functions.
(more…)