Author Interviews, Clots - Coagulation, Emergency Care, Pulmonary Disease, Stanford / 18.08.2018
Some Pulmonary Embolism Patients Can Be Treated at Home
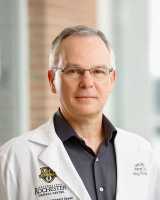
MedicalResearch.com Interview with:
Joseph Bledsoe MD, FACEP
Clinical Assistant Professor of Emergency Medicine
Stanford Medicine
Director of Research
Department of Emergency Medicine
Intermountain Medical Center
Murray, UT 84157
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Patients with blood clots in the lungs (pulmonary embolism) (PE) are routinely admitted to the hospital for blood thinning medications in the United States. However, evidence from other countries has shown that with appropriate risk stratification patients may be safe for outpatient treatment for their PE.
Our study is the largest prospective management study in the US to evaluate home treatment of patients with acute pulmonary embolism. We enrolled 200 patients and after risk stratification with the PE severity index score, leg ultrasounds and echocardiograms performed in the emergency department, patients were treated with blood thinning medications at home with routine outpatient follow up.
During the 90 day follow up period we found only one patient suffered a bleeding event after a traumatic injury, without any cases of recurrent symptomatic blood clots or death. (more…)

























![MedicalResearch.com Interview with: Dr. Theodore Satterthwaite MD Assistant professor in the department of Psychiatry, and Cedric Xia, a MD-PhD candidate Perelman School of Medicine at the University of Pennsylvania MedicalResearch.com: What is the background for this study? What are the main findings? Response: Unlike other branches of modern medicine, psychiatry still solely replies on patient reports and physician observations for clinical decision-making. Without biologically-based tests, the diagnostic categories for mental health do not carve nature at its joint. This is evident in the high levels of co-morbidity across disorders and heterogeneity within disorders. Through this research, we studied a large sample of adolescents who completed MRI-based functional imaging, and used recently-developed machine learning techniques to uncover specific abnormalities that are highly predictive of a wide variety of psychiatric symptoms. Essentially, we tried to find brain patterns that were predictive of different types of psychiatric symptoms. We discovered four such brain-guided dimensions of psychopathology: mood, psychosis, fear, and disruptive behavior. While each of these dimensions exhibits a unique pattern of brain connectivity, a common feature of brain anomaly is shared across the dimensions. Notably, in all linked dimensions, the default mode network and fronto-parietal network, two brain regions that usually become increasingly distinct as the brain matures, were abnormally connected. This loss of normal brain network segregation supports the hypothesis that many psychiatric illnesses may be disorders of brain development. MedicalResearch.com: What should readers take away from your report? Response: This study shows that we can start to use the brain to guide our understanding of psychiatric disorders in a way that’s fundamentally different than grouping symptoms into clinical diagnostic categories. By moving away from clinical labels developed decades ago, we can begin to let the biology speak for itself. Our ultimate hope is that understanding the biology of mental illnesses will allow us to develop better treatments for our patients. MedicalResearch.com: What recommendations do you have for future research as a result of this work? Response: This study demonstrates the importance of incorporating vast amounts of biological data to study mental illness across clinical diagnostic boundaries. Moving forward, we hope to integrate genomic data in order to describe pathways from genes to brain to symptoms, which could ultimately be the basis for novel treatments for mental illness. MedicalResearch.com: Is there anything else you would like to add? Response: Future breakthroughs in brain science to understand mental illness requires large amount of data. While the current study takes advantage of one of the largest samples of youth, the size (n=999) remains dwarfed by the complexity of the brain. The neuroscience community is actively working towards collecting higher quality data in even larger samples, so we can validate and build upon the findings. Citation: Cedric Huchuan Xia, Zongming Ma, Rastko Ciric, Shi Gu, Richard F. Betzel, Antonia N. Kaczkurkin, Monica E. Calkins, Philip A. Cook, Angel García de la Garza, Simon N. Vandekar, Zaixu Cui, Tyler M. Moore, David R. Roalf, Kosha Ruparel, Daniel H. Wolf, Christos Davatzikos, Ruben C. Gur, Raquel E. Gur, Russell T. Shinohara, Danielle S. Bassett, Theodore D. Satterthwaite. Linked dimensions of psychopathology and connectivity in functional brain networks. Nature Communications, 2018; 9 (1) DOI: 10.1038/s41467-018-05317-y [wysija_form id="3"] [last-modified] The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.](https://medicalresearch.com/wp-content/uploads/Cross-clinical-diagnostic-categories.jpg)
![MedicalResearch.com Interview with: Dr. Theodore Satterthwaite MD Assistant professor in the department of Psychiatry, and Cedric Xia, a MD-PhD candidate Perelman School of Medicine at the University of Pennsylvania MedicalResearch.com: What is the background for this study? What are the main findings? Response: Unlike other branches of modern medicine, psychiatry still solely replies on patient reports and physician observations for clinical decision-making. Without biologically-based tests, the diagnostic categories for mental health do not carve nature at its joint. This is evident in the high levels of co-morbidity across disorders and heterogeneity within disorders. Through this research, we studied a large sample of adolescents who completed MRI-based functional imaging, and used recently-developed machine learning techniques to uncover specific abnormalities that are highly predictive of a wide variety of psychiatric symptoms. Essentially, we tried to find brain patterns that were predictive of different types of psychiatric symptoms. We discovered four such brain-guided dimensions of psychopathology: mood, psychosis, fear, and disruptive behavior. While each of these dimensions exhibits a unique pattern of brain connectivity, a common feature of brain anomaly is shared across the dimensions. Notably, in all linked dimensions, the default mode network and fronto-parietal network, two brain regions that usually become increasingly distinct as the brain matures, were abnormally connected. This loss of normal brain network segregation supports the hypothesis that many psychiatric illnesses may be disorders of brain development. MedicalResearch.com: What should readers take away from your report? Response: This study shows that we can start to use the brain to guide our understanding of psychiatric disorders in a way that’s fundamentally different than grouping symptoms into clinical diagnostic categories. By moving away from clinical labels developed decades ago, we can begin to let the biology speak for itself. Our ultimate hope is that understanding the biology of mental illnesses will allow us to develop better treatments for our patients. MedicalResearch.com: What recommendations do you have for future research as a result of this work? Response: This study demonstrates the importance of incorporating vast amounts of biological data to study mental illness across clinical diagnostic boundaries. Moving forward, we hope to integrate genomic data in order to describe pathways from genes to brain to symptoms, which could ultimately be the basis for novel treatments for mental illness. MedicalResearch.com: Is there anything else you would like to add? Response: Future breakthroughs in brain science to understand mental illness requires large amount of data. While the current study takes advantage of one of the largest samples of youth, the size (n=999) remains dwarfed by the complexity of the brain. The neuroscience community is actively working towards collecting higher quality data in even larger samples, so we can validate and build upon the findings. Citation: Cedric Huchuan Xia, Zongming Ma, Rastko Ciric, Shi Gu, Richard F. Betzel, Antonia N. Kaczkurkin, Monica E. Calkins, Philip A. Cook, Angel García de la Garza, Simon N. Vandekar, Zaixu Cui, Tyler M. Moore, David R. Roalf, Kosha Ruparel, Daniel H. Wolf, Christos Davatzikos, Ruben C. Gur, Raquel E. Gur, Russell T. Shinohara, Danielle S. Bassett, Theodore D. Satterthwaite. Linked dimensions of psychopathology and connectivity in functional brain networks. Nature Communications, 2018; 9 (1) DOI: 10.1038/s41467-018-05317-y [wysija_form id="3"] [last-modified] The information on MedicalResearch.com is provided for educational purposes only, and is in no way intended to diagnose, cure, or treat any medical or other condition. Always seek the advice of your physician or other qualified health and ask your doctor any questions you may have regarding a medical condition. In addition to all other limitations and disclaimers in this agreement, service provider and its third party providers disclaim any liability or loss in connection with the content provided on this website.](https://medicalresearch.com/wp-content/uploads/Cross-clinical-diagnostic-categories-200x180.jpg)




