MedicalResearch.com Interview with:
Dr. W. Benjamin Nowell, Ph.D.
Director of Patient-Centered Research
CreakyJoints, study co-author
Co-principal investigator of ArthritisPower
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Rheumatoid Arthritis (RA) can diminish patients’ work productivity and increase the risk of long-term disability, economic insecurity and worsening health, but limited research informs these issues. The purpose of our study was to examine associations between patients’ RA disease activity and their productivity and workplace support, using real-world data from the ArthritisPower research registry.
Our study looked at a sample of participants with RA who had a history of or current treatment with non-biologic and/or biologic disease-modifying antirheumatic drugs (DMARD) (n=296). Among the study sample, 74 percent had high disease activity (HDA) as determined by RAPID3 (>12), a common measure of disease activity in RA.
- High disease activity was associated with lower education (p<0.001) and higher likelihood of disability (9%, p<0.001) compared to those without high disease activity.
- Patients with HDA missed more days of work than non-HDA patients (mean: 6.1 vs 3.8 days, respectively; p=0.03), but non-HDA participants reported more days off due to medical appointments (2.6 vs 1.2 days, respectively) while HDA patients missed more days due to RA treatment side effects (mean: 0.5 vs 0.1 days, respectively).
- Based on scores from the Work Productivity and Activity Impairment (WPAI) questionnaire, RA seems to affect work productivity to a greater extent in participants with HDA than without (WPAI scores 5.3 and 3.3, respectively; p<0.001). Participants who were not currently employed reported having more physically demanding tasks (e.g. heavy load lifting) and less workplace flexibility (e.g. working from home) in their most recent paid position than currently employed participants.
- However, in a multivariate regression analysis, we found that participants who could request changes in work start and stop times on a daily basis were 2.9 (95% CI: 1.53, 5.46) times more likely to be unemployed (adjusting for age, disease activity, and satisfaction with social participation) than those unable to make this request (p<0.0001).
About ArthritisPower: Created by
CreakyJoints and supported by a multiyear, multimillion dollar investment by the Patient-Centered Outcomes Research Institute (PCORI),
ArthritisPower is the first-ever patient-centered research registry for joint, bone, and inflammatory skin conditions. The free ArthritisPower mobile and desktop application allows patients to track and share their symptoms and treatments while also participating in voluntary research studies in a secure and accessible manner. ArthritisPower Patient Governors serve as gatekeepers for researchers who seek access to registry data or solicit the community to participate in unique, voluntary studies. To learn more and join ArthritisPower, visit
www.ArthritisPower.org.
(more…)


















 Dr. Wanpen Vongpatanasin, M.D.
Professor of Medicine
Program Director, Hypertension Fellowship Program
UT Southwestern Medical Center in Dallas
MedicalResearch.com: What is the background for this study? What are the main findings?
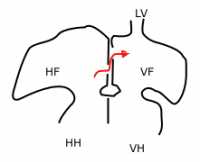
Response: The new US hypertension guideline places a greater emphasis on out-of-office blood pressure measurement, and maintains that a clinic BP of 130/80 mm Hg is equivalent to the same reading for home BP monitoring or daytime ambulatory BP monitoring. That is based, however, on data from non-US cohorts, primarily from Japanese cohorts and some European populations. None has been studied in the US population until now.
To find out, we analyzed large multi-ethnic studies of primarily young and middle-aged adults in Dallas, Texas, and Durham, N.C., that compared home blood pressure to clinic measurements, using the regression correlation (i.e. regression approach). To confirm the findings, we use another approach called “outcome approach” by determining risks of stroke, MI, and death associated with a clinic systolic blood pressure reading of 130 mmHg from the 3,132 participants in the Dallas study during an 11-year follow up.
Then, we determined the home blood pressure levels that carried the same heart disease risk and stroke risk as the clinic systolic 130 mm Hg reading.
We found that the level of home blood pressure of 130/80 mm Hg actually best correlates with blood pressure taken at the doctor’s office of 130/80 mmHg. This is true for whites, blacks and Hispanic patients in both treated and untreated population.
Dr. Wanpen Vongpatanasin, M.D.
Professor of Medicine
Program Director, Hypertension Fellowship Program
UT Southwestern Medical Center in Dallas
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: The new US hypertension guideline places a greater emphasis on out-of-office blood pressure measurement, and maintains that a clinic BP of 130/80 mm Hg is equivalent to the same reading for home BP monitoring or daytime ambulatory BP monitoring. That is based, however, on data from non-US cohorts, primarily from Japanese cohorts and some European populations. None has been studied in the US population until now.
To find out, we analyzed large multi-ethnic studies of primarily young and middle-aged adults in Dallas, Texas, and Durham, N.C., that compared home blood pressure to clinic measurements, using the regression correlation (i.e. regression approach). To confirm the findings, we use another approach called “outcome approach” by determining risks of stroke, MI, and death associated with a clinic systolic blood pressure reading of 130 mmHg from the 3,132 participants in the Dallas study during an 11-year follow up.
Then, we determined the home blood pressure levels that carried the same heart disease risk and stroke risk as the clinic systolic 130 mm Hg reading.
We found that the level of home blood pressure of 130/80 mm Hg actually best correlates with blood pressure taken at the doctor’s office of 130/80 mmHg. This is true for whites, blacks and Hispanic patients in both treated and untreated population. 








 Faiz Gani, PhD
Postdoctoral research fellow
Department of Surgery
Johns Hopkins University School of Medicine
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Firearm related injuries are a leading cause of injury and death in the United States, yet, due to combination of factors, limited data exist that evaluate these injuries, particularly among younger patients (patients younger than 18 years).
The objective of this study was to describe emergency department utilization for firearm related injuries and to quantitate the financial burden associated with these injuries.
In our study of over 75,000 emergency department visits, we observed that each year, over 8,300 children and adolescents present to the emergency department for the treatment / management of a gunshot injury. Within this sub-population of patients, we observed that these injuries are most frequent among patients aged 15-17 years and while these injuries decreased over time initially, were observed to increase again towards the end of the time period studied.
In addition to describing the clinical burden of these injuries, we also sought to describe the financial burden associated with these injuries. For patients discharged from the emergency department, the average (median) charge associated with their care was $2,445, while for patients admitted as inpatients for further care, the average (median) charge was $44,966.
Collectively these injuries resulted in $2.5 billion in emergency department and hospital charges over the time period studied. This translates to an annual financial burden of approximately $270 million.
Faiz Gani, PhD
Postdoctoral research fellow
Department of Surgery
Johns Hopkins University School of Medicine
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Firearm related injuries are a leading cause of injury and death in the United States, yet, due to combination of factors, limited data exist that evaluate these injuries, particularly among younger patients (patients younger than 18 years).
The objective of this study was to describe emergency department utilization for firearm related injuries and to quantitate the financial burden associated with these injuries.
In our study of over 75,000 emergency department visits, we observed that each year, over 8,300 children and adolescents present to the emergency department for the treatment / management of a gunshot injury. Within this sub-population of patients, we observed that these injuries are most frequent among patients aged 15-17 years and while these injuries decreased over time initially, were observed to increase again towards the end of the time period studied.
In addition to describing the clinical burden of these injuries, we also sought to describe the financial burden associated with these injuries. For patients discharged from the emergency department, the average (median) charge associated with their care was $2,445, while for patients admitted as inpatients for further care, the average (median) charge was $44,966.
Collectively these injuries resulted in $2.5 billion in emergency department and hospital charges over the time period studied. This translates to an annual financial burden of approximately $270 million.