Author Interviews, Brain Injury, University Texas / 24.06.2019
CTE Brain Pathology Found More Commonly in Former Athletes and Men
MedicalResearch.com Interview with:
Kevin F. Bieniek, Ph.D.
Assistant Professor, Department of Pathology & Laboratory Medicine
Joe R. & Teresa Lozano Long School of Medicine
Director, Biggs Institute Brain Bank Core
Glenn Biggs Institute for Alzheimer’s & Neurodegenerative Diseases
University of Texas Health Science Center San Antonio
San Antonio, Texas 78229
MedicalResearch.com: What is the background for this study? Would you briefly explain what is meant by CTE?
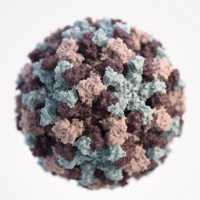
Response: CTE, or chronic traumatic encephalopathy, is a progressive neurodegenerative disorder that is linked to prior exposure to repetitive traumatic brain injuries. CTE pathology, characterized by a distinct deposition pattern of the protein ‘tau’, is most often observed in the brains former contact sport athletes and military veterans. The public health impacts of this disorder are largely unknown, as this disease is often studied in individuals which advanced levels of exposure, particularly professional American football player.
This study aimed to understand what the presence of this disorder might be in the general population by studying athletes and non-athletes, a number of different sports, different levels of participation, and both males and females.
(more…)