Author Interviews, Brigham & Women's - Harvard, Heart Disease, Nature / 04.02.2021
AI Can Generate Predictive Coronary Calcium Score in Two Seconds
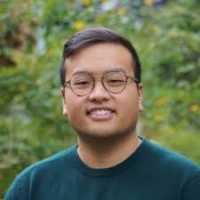
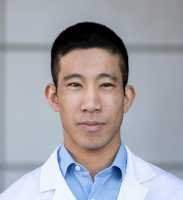
MedicalResearch.com Interview with:
Dr. Hugo Aerts, PhD
Dana-Farber Cancer Institute
Associate Professor, Brigham and Women's Hospital
Harvard Medical School
Director, Program for Artificial Intelligence in Medicine
Brigham And Women's Hospital
MedicalResearch.com: Deep convolutional neural networks to predict cardiovascular risk from computed tomography
Response: Cardiovascular disease is the most common preventable cause of death in Europe and the United States. Effective lifestyle and pharmacological prevention is available, but identifying those who would benefit most remains an ongoing challenge. Hence, efforts are needed to further improve cardiovascular risk prediction and stratification on an individual basis.
One of the strongest known predictors for adverse cardiovascular events is coronary artery calcification, which can be quantified on computed tomography (CT). The CT coronary calcium score is a measure of the burden of coronary atherosclerosis and is one of the most widely accepted measures of cardiovascular risk.
Recent strides in artificial intelligence, deep learning in particular, have shown its viability in several medical applications such as medical diagnostic and imaging, risk management, or virtual assistants. A major advantage is that deep learning can automate complex assessments that previously could only be done by radiologists, but now is feasible at scale with a higher speed and lower cost. This makes deep learning a promising technology for automating cardiovascular event prediction from imaging. However, before clinical introduction can be considered, generalizability of these systems needs to be demonstrated as they need to be able to predict cardiovascular events of asymptomatic and symptomatic individuals across multiple clinical scenarios, and work robustly on data from multiple institutions.
(more…)