Alzheimer's - Dementia, Author Interviews, Cognitive Issues, Obstructive Sleep Apnea, Pulmonary Disease, University of Michigan / 16.04.2021
Sleep Apnea: CPAP Therapy May Reduce Risk of Dementia
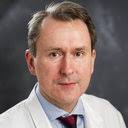
MedicalResearch.com Interview with:
Galit Levi Dunietz MPH, PhD
Assistant Professor
University of Michigan, Medical School
Department of Neurology
Department of Nutritional Sciences
Ann Arbor, MI 48109-5845
MedicalResearch.com: What is the background for this study?
Response: Dementia is a public health crisis that affects more than 6 million Americans. As no treatments to effectively reverse dementia are currently available, interest has shifted toward modifiable risk factors for dementia, which may offer a critical window for prevention or intervention.
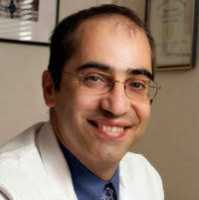
Recent research suggests that obstructive sleep apnea (OSA) is a common, yet undiagnosed, risk factor for cognition impairment in older adults. However, few studies have examined whether treatment of OSA with positive airway pressure (PAP) therapy could protect those with OSA against developing dementia, says principal investigator, Dr. Tiffany Braley, MD, MS, Associate Professor of Neurology from the University of Michigan.
To address this gap, Dr. Braley and Dr. Galit Levi Dunietz, PhD, MPH, Assistant Professor and sleep epidemiologist, examined associations between PAP therapy use and 3-year incidence of Alzheimer’s disease, mild cognitive impairment (MCI), or other forms of dementia (DNOS, “dementia not otherwise specified”).
(more…)
Tiffany Braley, MD, MS Associate Professor