AHA Journals, Author Interviews, Blood Pressure - Hypertension, Toxin Research, University of Michigan / 26.10.2018
Low Level Lead Exposure Linked to Resistant Hypertension
MedicalResearch.com Interview with:
Sung Kyun Park Sc.D. M.P.H.
Associate professor of epidemiology and environmental health sciences
University of Michigan School of Public Health
Ann Arbor, Michigan
MedicalResearch.com: What is the background for this study? What are the main findings?
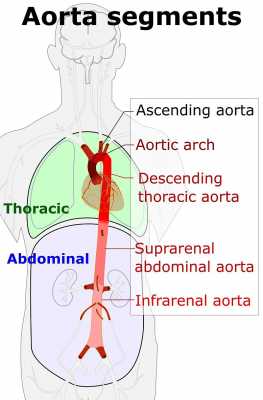
Response: It is poorly understood that why some patients need more drugs to control high blood pressure than others. Resistant hypertension is that blood pressure is not controlled with 3 medications of different classes including diuretics or is required 4 or more medications of different classes for blood pressure controls. Genes, obesity, physical inactivity, high salt diet, pain medications may do something. Lead is a widespread environmental toxin that can influence high blood pressure. In this study, we examined whether long-term exposure to lead, measured as bone lead, is associated with the risk of resistant hypertension.
Bone lead offers a better method over blood lead measurement to discern long-term lead exposure and accumulation.
The main finding of our study is that low-level lead exposure, measured in the tibia (hard bone), is associated with higher risk of development of resistant hypertension in a cohort of patients diagnosed with hypertension. (more…)



 Jennifer Woo Baidal, MD, MPH
Assistant Professor of Pediatrics
Director of Pediatric Weight Management,
Division of Pediatric Gastroenterology, Hepatology, and Nutrition,
Columbia University Medical Center &
New York-Presbyterian Morgan Stanley Children’s Hospital
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Childhood obesity prevalence is historically high, with most incident obesity among children occurring before age 5 years. Racial/ethnic and socioeconomic disparities in childhood obesity are already apparent by the first years of life. Latino/Hispanic children in low-income families are at-risk for obesity. Thus, understanding potentially effective ways to prevent childhood obesity, particularly in vulnerable populations, should focus on early life.
Sugar-sweetened beverage (SSB) consumption is a modifiable risk factor for obesity and is linked to other adverse health outcomes. Maternal SSB consumption in pregnancy and infant sugar-sweetened beverage consumption in the first year of life are linked to later childhood obesity.
We sought to describe beverage consumption in a modern cross-sectional cohort of 394 low-income, Latino families, and to examine the relationship of parental attitudes toward sugar-sweetened beverages with parental and infant SSB consumption.
Jennifer Woo Baidal, MD, MPH
Assistant Professor of Pediatrics
Director of Pediatric Weight Management,
Division of Pediatric Gastroenterology, Hepatology, and Nutrition,
Columbia University Medical Center &
New York-Presbyterian Morgan Stanley Children’s Hospital
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: Childhood obesity prevalence is historically high, with most incident obesity among children occurring before age 5 years. Racial/ethnic and socioeconomic disparities in childhood obesity are already apparent by the first years of life. Latino/Hispanic children in low-income families are at-risk for obesity. Thus, understanding potentially effective ways to prevent childhood obesity, particularly in vulnerable populations, should focus on early life.
Sugar-sweetened beverage (SSB) consumption is a modifiable risk factor for obesity and is linked to other adverse health outcomes. Maternal SSB consumption in pregnancy and infant sugar-sweetened beverage consumption in the first year of life are linked to later childhood obesity.
We sought to describe beverage consumption in a modern cross-sectional cohort of 394 low-income, Latino families, and to examine the relationship of parental attitudes toward sugar-sweetened beverages with parental and infant SSB consumption.




 Dr. Janey Pratt, MD
Clinical Associate Professor, Surgery
Stanford University
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: In 2013 obesity became recognized as a disease. The rate of pediatric obesity continues to rise. Severe pediatric obesity is rising at a even faster rate than obesity in pediatrics. Despite this Metabolic and Bariatric Surgery (MBS) remains underutilized in the treatment of severe pediatric obesity. There is a significant amount of adult data and now pediatric data about effective treatments for severe obesity. These support the use of MBS as a primary treatment for severe obesity in children. (BMI > 120% of 95th percentile with a comorbidity or BMI > 140% of 95th percentile).
Dr. Janey Pratt, MD
Clinical Associate Professor, Surgery
Stanford University
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: In 2013 obesity became recognized as a disease. The rate of pediatric obesity continues to rise. Severe pediatric obesity is rising at a even faster rate than obesity in pediatrics. Despite this Metabolic and Bariatric Surgery (MBS) remains underutilized in the treatment of severe pediatric obesity. There is a significant amount of adult data and now pediatric data about effective treatments for severe obesity. These support the use of MBS as a primary treatment for severe obesity in children. (BMI > 120% of 95th percentile with a comorbidity or BMI > 140% of 95th percentile).


 Kathryn M. Edwards, M.D.
Sarah H. Sell and Cornelius Vanderbilt Chair in Pediatrics
Professor of Pediatrics
Vanderbilt University School of Medicine
Dr. Edwards discusses the statement from the Infectious Diseases Society of America (IDSA) regarding the Centers for Disease Control and Prevention’s new data on child vaccine rates across the United States.
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: To monitor the uptake of vaccines the CDC conducts a National Immunization Survey each year. This survey is conducted by random-digit dialing (cell phones or landlines) of parents and guardians of children 19-35 months of age. The interviewers ask the families who provides the vaccines for their children and if these providers can be contacted to inquire about the immunizations received. The overall response rate to the telephone survey was 26% and immunization records were provided on 54% of the children where permission was granted. Overall 15, 333 children had their immunization records reviewed.
When comparing immunization rates for 2017 and 2016, the last two years of the study, several new findings were discovered.
First the overall coverage rate for 3 doses of polio vaccine, one dose of MMR, 3 doses of Hepatitis b, and 1 dose of chickenpox vaccine was 90%, a high rate of coverage. Children were less likely to be up to date on the hepatitis A vaccine (70%) and rotavirus vaccine (73%). Coverage was lower for children living in rural areas when compared with urban areas and children living in rural areas had higher percentages of no vaccine receipt at all (1.9%) compared with those living in urban areas (1%).
There were more uninsured children in 2017 at 2.8% and these children had lower immunization rates. In fact 7.1% of the children with no insurance were totally unimmunized when compared with 0.8% unimmunized in those with private insurance. Vaccine coverage varies by state and by vaccine.
Kathryn M. Edwards, M.D.
Sarah H. Sell and Cornelius Vanderbilt Chair in Pediatrics
Professor of Pediatrics
Vanderbilt University School of Medicine
Dr. Edwards discusses the statement from the Infectious Diseases Society of America (IDSA) regarding the Centers for Disease Control and Prevention’s new data on child vaccine rates across the United States.
MedicalResearch.com: What is the background for this study? What are the main findings?
Response: To monitor the uptake of vaccines the CDC conducts a National Immunization Survey each year. This survey is conducted by random-digit dialing (cell phones or landlines) of parents and guardians of children 19-35 months of age. The interviewers ask the families who provides the vaccines for their children and if these providers can be contacted to inquire about the immunizations received. The overall response rate to the telephone survey was 26% and immunization records were provided on 54% of the children where permission was granted. Overall 15, 333 children had their immunization records reviewed.
When comparing immunization rates for 2017 and 2016, the last two years of the study, several new findings were discovered.
First the overall coverage rate for 3 doses of polio vaccine, one dose of MMR, 3 doses of Hepatitis b, and 1 dose of chickenpox vaccine was 90%, a high rate of coverage. Children were less likely to be up to date on the hepatitis A vaccine (70%) and rotavirus vaccine (73%). Coverage was lower for children living in rural areas when compared with urban areas and children living in rural areas had higher percentages of no vaccine receipt at all (1.9%) compared with those living in urban areas (1%).
There were more uninsured children in 2017 at 2.8% and these children had lower immunization rates. In fact 7.1% of the children with no insurance were totally unimmunized when compared with 0.8% unimmunized in those with private insurance. Vaccine coverage varies by state and by vaccine.